What Are Cord Blood Stem Cells?
Umbilical Cord blood ("UCB") is the blood found in the umbilical cord and placenta following the birth of a baby after the umbilical cord is cut. It is a rich source of stem cells that are being used today to treat various serious diseases.
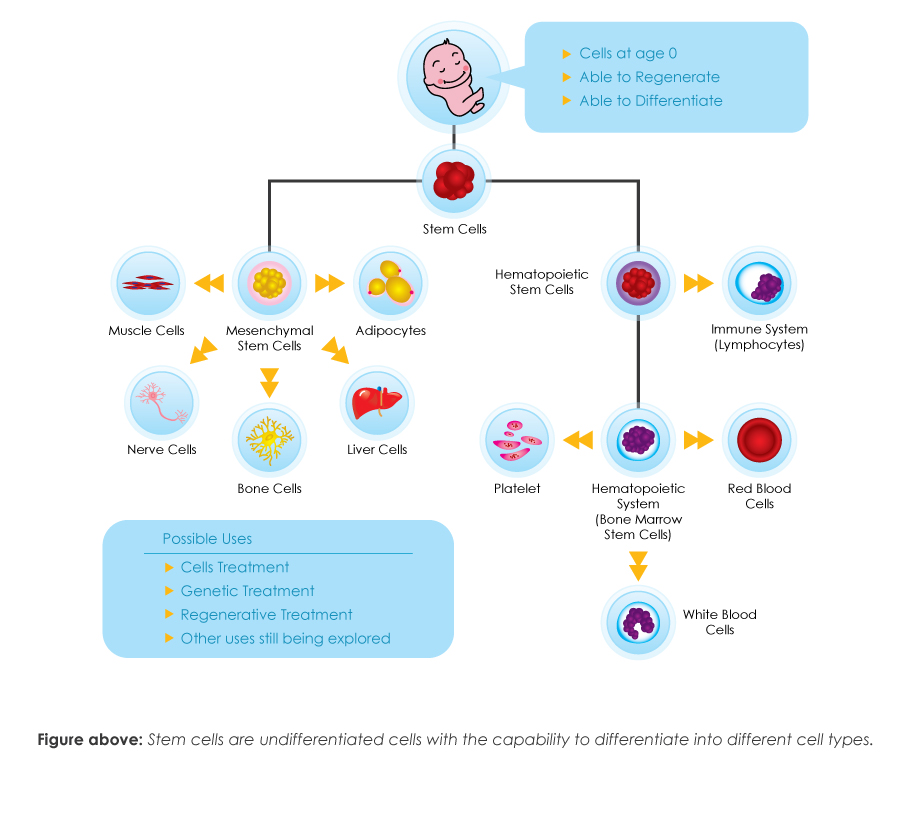
Stem cells are the master cells of the body, the building blocks of tissues and organs. They have been described as young, undifferentiated, “magical” cells that can be developed into other types of cells.
UCB, once regarded as biological waste, is now highly regarded as a very precious therapeutic resource and can be collected in a safe manner by obstetrician or midwife following the birth of the baby.
Why cord blood banking?
Why is It Important to Save Your Baby’s Cord Blood?
- It is an Once-in-a-Lifetime Opportunity to store and protect your child in the future.
Store your baby's umbilical cord blood is once In-a-Lifetime opportunity after your baby is delivered. Your baby's umbilical cord blood is rich sources of stem cells. These cells are genetically unique to each person and have the ability to renew and replace cells in the blood, tissues, organs, and immune system. - It is a form of bio-insurance for the family.
Today, you store your baby's cord blood is a potential medical resource for the future, and does not require stringent matching as opposed to conventional bone marrow stem cell transplants. Within the family, there is about 70% of patients who need a transplant are unable to find a suitable match. - Ease of collection, which is pain-free and risk-free to both mother and child.
Collection of cord blood is a relatively easy task, which is handled by your own delivering doctor. There is no affect during the birthing process. - It offers you the advantages of potentially treating various life threatening diseases.
Based on the statistics have shown, there is 1 in every 217 persons may need stem cells for treatment in their lifetime2. Your baby's cord blood contains a rich source of such stem cells. Since 1988, doctors have used cord blood stem cells to treat more than 30,000 patients3 suffering from diseases such as leukaemia, other cancers, blood disorders and in other clinical trials. - Less risk of transplant rejection (Graft vs. Host Disease (GVHD)).
The term of Graft vs. Host Disease refers to a common complication where the transplanted tissue attacks the patient's own tissue. This disease will usually occur in transplants when the donor and recipient are different.
Today, cord blood stem cells are used in the treatment of nearly 80 diseases, including blood disorders, immune system deficiencies, metabolic disorders, bone marrow failure syndromes, a wide range of cancers, and tumours such as neuroblastoma, which can be treated with cord blood stem cell transplant therapy. Studies have shown that at least 50% of childhood cancer incidences can similarly be treated.
In a cord blood transplant, stem cells are infused into a patient's bloodstream where they heal and repair damaged cells and tissues. When a transplant is successful, a new healthy immune system is created. With is great therapeutic potentials, cord blood banking has become very popular and has become a very plausible option for parents who wish to provide an added security for their loved ones.
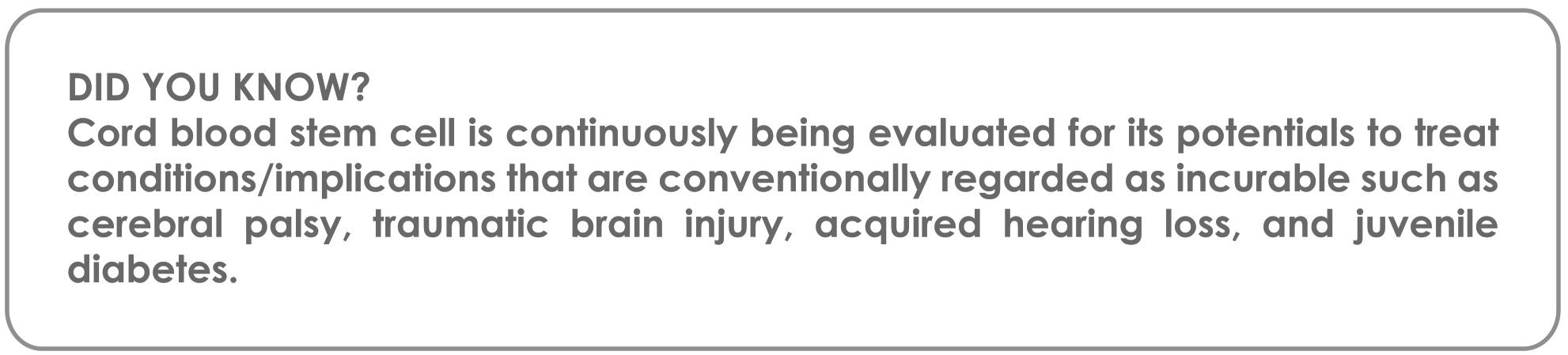
Diseases Potentially Treatable By Stem Cells
Comparison of Different Sources of Stem Cells
| Cord Blood Stem Cell | Wharton's Jelly MSC | Adipose Derived MSC | |
|---|---|---|---|
| Source | Placenta and umbilical cord | Umbilical Cord | Adipose tissue under skin |
| Harvest Process | Harvested from the placenta and umbilical cord during birth | Harvested through enzymatic digestion of the outer layer of umbilical cord | Harvest through operation |
| Chances of disease transmission | Lowest | Lowest | Lowest |
| Cell culture proliferation | High | High | High |
| Risk of transplant (Graft vs Host disease) | Lowest | Lower | Lower |
| Side effects to donor | Non-invasion (Not harmful to mother or child) | Non-invasion (Not harmful to mother or child) | Invasive (skin is penetrated to reach adipose tissue) |
| Difficulty of collection | No risk or pain imposed | No risk or pain imposed | Causes nausea |
CORD BLOOD COLLECTION
How is Cord Blood Collected?
UCB is harvested from the cord once the cord has been clamped and cut. UCB is collected into a bag and will go for further processing (primarily to remove red blood cells) before it is permanently cryopreserved in a liquid nitrogen freezer for potential use at a later time. Collection of the UCB is fast, safe, and posses no risk or pain for the mother or the newborn. It also does not interfere with the birth process. UCB can be collected safely regardless of natural, caesarean or water birth, and it does not affect the flow of oxygen to your baby.
It is however important to note that the collection of the UCB is secondary to any medical issues that may arise during the birth of your child. As such, the decision to proceed with cord blood collection lies at the sole discretion of your obstetrician or midwife.
How Much Cord Blood Could Be Collected From My Baby’s Umbilical Cord?
The quantity of cord blood collected varies from baby to baby. On an average, about 60 – 75 ml of cord blood can be collected from an Asian baby. However, the important factor is not the volume of the blood collected but the number of nucleated cells harvested after the processing of the cord blood. Scientists around the world have achieved progress in the stem cell expansion field so even cord blood units with low cells counts may prove to be useful in the future.
Other Than Cord Blood, What else Would Be Collected?
Samples of the maternal blood are drawn after the delivery process. The maternal blood will be tested for a list of infectious diseases, including HIV, Hepatitis B and C, Cytomegalovirus, and Syphilis. These tests are the basic requirement in international cord blood cryopreservation standard so as to determine the safety and quality of the collected cord blood unit.
Why Does Cord Blood Need To Be Processed After It Is Collected?
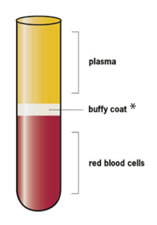
The three main types of cells in cord blood are red blood cells, white blood cells and plasma. The heaviest layer is the red blood cells, the lightest is the plasma, and in the middle is a pinkish layer called the ‘buffy coat’, which contains the white blood cells – including stem cells. Thus, cord blood needs to be processed after it is collected so that stem cells could be harvested.
The processing method is hence the key to acquiring/harvesting quality cord blood stem cells. At Cellsafe, our superior processing technology and know-how assures that get the best results in terms of recovery and viability of all our samples.

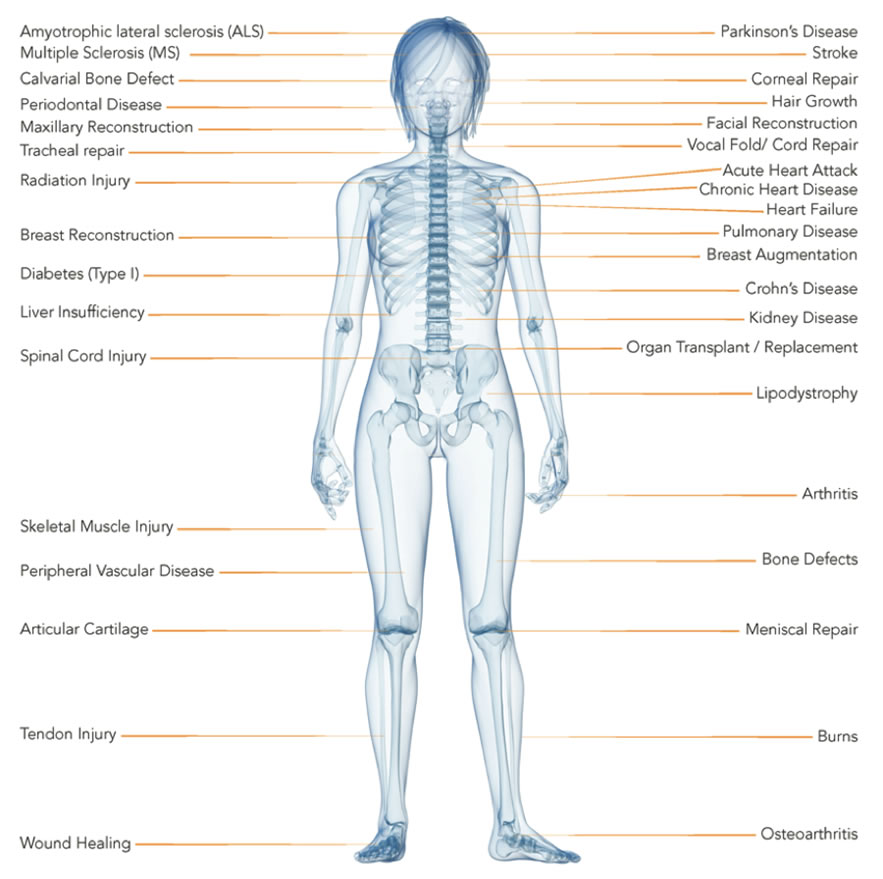
The Storage of Cord Blood Stem Cells
Each of the cord blood unit that reaches Cellsafe is given a unique identifying tag that is tracked by our proprietary computer systems at all times.
Once the cord blood is processed, the cord blood stem cells are placed in FDA-approved freezing bags. Each FDA-approved freezing bag is clearly marked with your baby’s name, date of birth, date of processing and contents as well as a unique Identifying Number.
The freezing bag is then frozen at a computer-controlled rate to a storage temperature of -150°C. The frozen cord blood stem cells are stored in liquid nitrogen tanks located in a constantly monitored and secure laboratory facility.
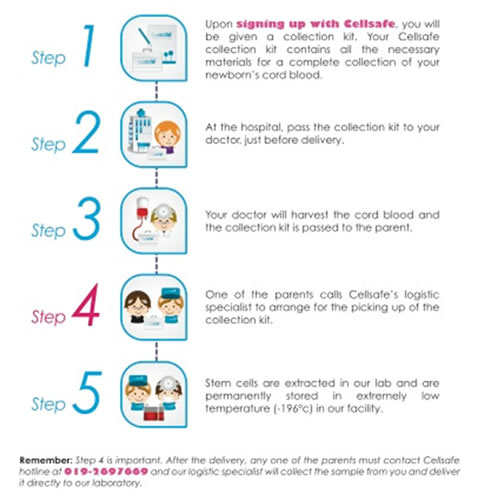
HOW TO SAVE CORD BLOOD
Simple Steps to Save Cord Blood
WHO COULD USE MY BABY’S CORD BLOOD?
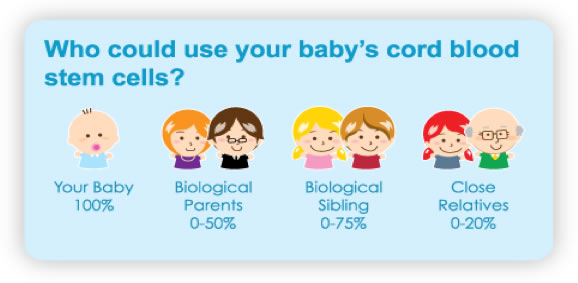
Who Could Use Your Baby's Cord Blood Stem Cells?
- Your baby
- Biological siblings
- Biological parents
- Close relatives
The stem cells from your baby's cord blood are a great perfect match with him/her. When you cryopreserved these stem cells, you are also keeping a ready source of genetically related stem cells for someone else in the family. The chances of locating a match within the family can be as high as 40%.
Cord blood does not have to be as closely matched as bone marrow or peripheral blood transplants typically require a 6/6 HLA match but a closely matched cord blood transplant is preferable since cord blood has been transplanted successfully with as low as a 3/6 HLA match.
 +603-4050 5509
+603-4050 5509